What Are Depression Resources And Services For Veterans

Co-ordinate to the National Plant of Mental Wellness (NIMH), one out of five adults in the United states of america lives with a mental affliction. When information technology comes to servicemembers, the National Alliance on Mental Illness (NAMI) notes that "nearly 1 in 4 active duty members showed signs of a mental health condition."
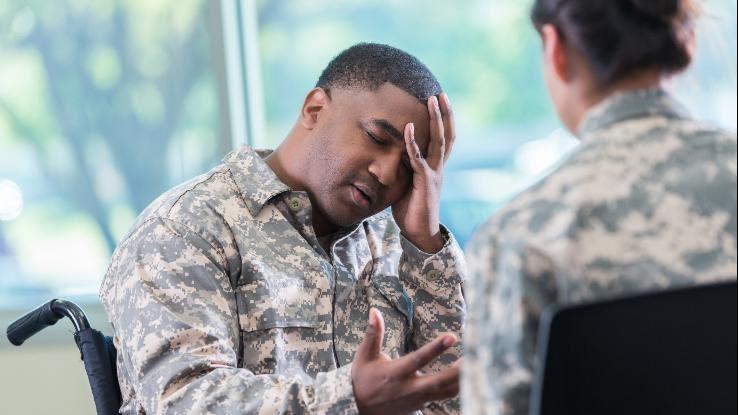
Whether a mental illness or disorder is augmented by, or newly triggered by, their experiences in the military, veterans demand more support when information technology comes to their mental health. The U.S. Department of Veteran Affairs (VA) reported that more than one.7 million veterans received treatment in a VA mental health program in 2018. While it's reassuring to hear that these vets have found the support and treatment they need, it'due south also clear that many veterans and active duty members are not supported — nor are they even aware of the ways they can seek assist.
To this terminate, the U.Due south. Government Accountability Part (GAO) constitute that veterans are 1.5 times more than likely to die by suicide. In add-on to suicidal ideation, veterans may likewise feel other mental illnesses or disorders, including post-traumatic stress disorder (PTSD), depression, traumatic brain injury (TBI) and substance use disorder (SUD).
Many of united states of america honor our servicemembers on Veterans Solar day with words of gratitude, parades and ceremonies, but it should not end there — and should not be bars to a single twenty-four hour period. All yr long, yous tin find ways to back up veterans with mental illnesses and disorders. The first step? Educating yourself. Here, we will take a deeper look at some of the near common mental wellness concerns vets navigate daily.
Post-Traumatic Stress Disorder (PTSD)
Postal service-traumatic stress disorder (PTSD) develops after someone experiences a shocking, frightening and/or unsafe event. As y'all can imagine, PTSD is mutual among frontline vets and agile duty soldiers who have seen combat. Triggers can include, but are not limited to, the following:
- Witnessing the deaths of beau armed forces personnel or civilians
- Life-threatening injuries
- Lack of back up from friends and family after retirement
During a traumatic event, our bodies react in a variety of means to protect united states of america from danger. Some people will struggle with anxiety immediately post-obit their traumatic experience, but, over time, those feelings will lessen. However, people diagnosed with PTSD proceed to be traumatized by the experience, and often experience stressed or frightened even when they are non in danger.
Our bodies are incredibly well-equipped when information technology comes to keeping us rubber; if we perceive danger, our fight-or-flight instincts kick in. When y'all experience a specially traumatizing event, information technology can be challenging to convince yourself — and your body — that you're no longer in danger. After all, anxiety does not mind to reason.
According to the American Psychiatric Association, mutual PTSD symptoms, which can often assistance a doctor in formulating a diagnosis, tin can be grouped into the post-obit four categories:
Intrusion
Alternatively known as re-experiencing symptoms, these intrusive thoughts are incredibly vivid and come in the form of "involuntary memories; lamentable dreams; or flashbacks of the traumatic event." No matter the type of intrusion, this symptom makes veterans feel similar they are reliving the triggering traumatic experience all over once again.
Avoidance
While some veterans might find sharing their gainsay stories cathartic, others do not enjoy recalling their time on the ground. These memories tin can cause unexpected emotions and reactions, which might atomic number 82 a vet to avert places, people and things that remind them of the inciting traumatic outcome; they may also withdraw from conversations surrounding the military or their service time. While some veterans may exist witting of their avoidance, others may non realize they're doing so. No matter their level of awareness, veterans often have difficulty seeking back up or treatment because they rather avoid a chat — fifty-fifty a well-intentioned ane — than relive a traumatic experience.
Alterations in Cognition and Mood
Undoubtedly, there's a link between emotion and cognition. Emotional Intelligence (EI) is your ability to empathise, use, perceive, and control their emotions, while cognition is your power to gain cognition, understand it, and react to it by making an appropriate decision. Some veterans may experience a cognitive bias — that is, they'll put an excessive amount of their time, attending and energy into mitigating perceived threats.
For instance, during their fourth dimension in the service, a vet may have seen a beau soldier die as a result of someone's determination-making. That said, this will stick with them, fifty-fifty if there isn't a direct correlation between a decision and the traumatic outcome. Once habitation, vets might perceive everyday activities every bit unsafe and they'll stay "on guard" to prevent a future traumatic effect or threat, fifty-fifty if one doesn't exist.
Alterations in Arousal and Reactivity
Also known every bit "hyper-vigilance," this symptom is marked by enhanced awareness, which can turn into reckless beliefs. Vets might be more hands agitated or have difficulty sleeping. Much like the feeling of being "on guard," vets will often say alert because their bodies are anticipating danger. Information technology'southward like beingness unable to plow off your fight-or-flight instinct. Living with all that doubt tin can pb vets to engage in cocky-harming behaviors.
Depression (Major Depressive Disorder)
Low, or major depressive disorder, is marked by extreme sadness and feelings of hopelessness, which impact not merely your mood, but your thoughts and actions as well. While almost people feel sadness or depressive episodes, those who have been diagnosed with depression find these feelings of hopelessness and sadness interfering with, and inhibiting, their mean solar day-to-day lives.

Veterans with PTSD are probable to feel depression every bit a comorbidity — a concurrent condition. Veterans and other people with depression might experience the following symptoms:
- Feeling sad or depressed for a sustained length of fourth dimension
- Loss of interest in activities y'all one time enjoyed
- Changes in appetite
- Changes in weight
- Trouble falling or staying asleep
- Sleeping too much
- Loss of free energy or fatigue
- Inability sit withal
- Feelings of worthlessness or guilt
- Difficulty concentrating or making decisions
- Suicidal thoughts or ideation
Sometimes these symptoms go undiagnosed or, due to the diagnostic requirements, a veteran may be living with depression for months or years before they receive a proper diagnosis and treatment. If the disorder remains underlying, veterans and other people with depression may experience worsening symptoms, including increased suicidal thoughts. The VA approximates that betwixt 18–22 veterans a day dice past suicide. Regardless of the symptoms a veteran is experiencing as a result of major depressive disorder, finding support is essential to learning how to better manage their day-to-solar day lives.
Traumatic Brain Injury (TBI)
While a traumatic brain injury (TBI) is oft caused by a physical, outside force, information technology affects how your brain functions, which can lead to accompanying mental affliction or disorders. "The Defense and Veterans Brain Injury Eye (DVBIC) reported nearly 414,000 TBIs among U.Southward. service members worldwide between 2000 and late 2019," the VA notes. "More 185,000 Veterans who utilise VA for their health care have been diagnosed with at least one TBI."

As mentioned, TBIs result from a significant blow to the caput or body. According to the U.S. Section of Defense, 1% of vets suffered from severe cases, while 9.1% suffered from moderate cases of the status. The remaining 82.4% suffered from mild cases.
While TBI and PTSD share several symptoms, the 2 conditions are non the same. TBI stems from a combat-related incident, which means the diagnosis is generally concurrent. Veterans with a TBI may feel the post-obit:
- Difficulty maintaining intimate relationships
- Personality changes, such as varying mood swings
- Low
- Motor impairment
Substance Use Disorder (SUD)
Substance use disorder (SUD), which is sometimes referred to as addiction, tin can impact a person's physical and mental wellbeing. For many, the mode a substance changes their brain and behavior leads to an disability to control their substance use. The VA reports that of the vets returning from tours in Iraq and Transitional islamic state of afghanistan, x% have a substance abuse disorder involving either drugs or alcohol.

While it's not always the instance, veterans with substance corruption disorder may also feel depression or PTSD. Co-ordinate to the VA, ane third of vets seeking treatment for SUD too have PTSD. Veterans and other people with substance abuse disorder may experience the following symptoms:
- An intense urge to use the substance/drug regularly — daily or several times a day — that blocks out other thoughts
- Needing to take larger amounts of the substance to achieve the desired upshot
- Unsustainably spending coin on the substance
- Inability to deliver on obligations and piece of work tasks
- Retreating from social activities
- Using the substance even if y'all know information technology's causing you damage
- Experiencing withdrawal symptoms when y'all finish taking the substance
- The substance — needing to become it, accept it, use it, recover from information technology — interferes with your ability to office or perform other daily activities
- Inability to stop using the substance
- Periods of binge drinking
- Dumb judgement
- Mood swings
- Low
- Negatively impacting those around y'all or an inability to maintain relationships
Knowing how to offer support to a loved i with a substance use disorder can be challenging. For many people, not just vets, drugs and alcohol tin provide a means of temporary "escape" from depressive episodes, intrusive thoughts, anxiety or trauma. As a form of cocky harm, it often provides in-the-moment relief, which makes information technology hard for the person with a substance utilize disorder to end using the substance.
This can be complicated by comorbidities, such equally PTSD and depression: SUD, like all other mental illnesses, has a stigma attached to it; oftentimes, people blame the person with the substance use disorder. When these stigmas — and the accompanying feelings of guilt and shame — compound, seeking support and handling becomes that much harder.
How Tin can Y'all Support Veterans with Mental Illnesses and Disorders?
Although some service members may seek handling from a nonmilitary healthcare provider, the VA, or U.S. Department of Veterans Matter, is a federal department charged with providing life-long healthcare services to veterans. With roughly one,700 VA medical centers and clinics throughout the country, the department ensures vets receive the back up and treatment they need for both their physical and mental health.
Despite the VA's all-time efforts, however, our healthcare system is yet lacking. According to the National Quango for Mental Wellbeing, "less than 50% of returning veterans in demand receive any mental wellness treatment." While more people are speaking out about their mental health and mental illnesses, there'southward still a stigma — and that stigma often prevents vets (and all of u.s.a.) from seeking treatment or support. In fact, this stigma tin also lead to a lack of education; often, people don't know what they're experiencing when symptoms of a mental illness or disorder begin.

So, how tin we start to change this harmful condition quo? The first footstep might merely be educating veterans — and all people — on the importance of mental wellness. Simply equally you'd seek handling for a concrete injury or illness, you should feel comfy seeking treatment for a mental affliction, as well. You can too help advocate for better standards of care for our vets as well every bit an increased number of trained mental healthcare providers who are both accessible and well-versed in the specific needs vets may take when seeking support.
Resource Links:
- "Mental Illness" via National Institute of Mental Wellness (NIMH)
- "Veterans' Growing Need for Mental Wellness Services" via U.Due south. Government Accountability Office (GAO)
- "Mental Health" via U.Due south. Department of Veteran Affairs (VA)
- "Veterans & Active Duty: Mental Health Concerns" via National Alliance on Mental Illness (NAMI)
- "Postal service-Traumatic Stress Disorder" via National Establish of Mental Health (NIMH)
- "What Is PTSD?" via American Psychiatric Clan
- "What Is Low?" via American Psychiatric Association
- "Traumatic Brain Injury (TBI)" via U.S. Department of Veteran Affairs (VA)
- "PTSD and Substance Corruption in Veterans" via U.S. Department of Veteran Affairs (VA)
- "Substance Use Disorder" via Mayo Clinic
- "How to Offer Intervention Assistance in a Respectful & Supportive Way" via SymptomFind
- "Veterans" via National Council for Mental Wellbeing
- "The Missing Context Behind the Widely Cited Statistic That In that location Are 22 Veteran Suicides a Twenty-four hours" via The Washington Post
What Are Depression Resources And Services For Veterans,
Source: https://www.symptomfind.com/healthy-living/ptsd-and-other-mental-health-conditions-veterans?utm_content=params%3Ao%3D740013%26ad%3DdirN%26qo%3DserpIndex
Posted by: gonzalezwitepheres.blogspot.com


0 Response to "What Are Depression Resources And Services For Veterans"
Post a Comment